For decades, the world made steady progress toward one of the most ambitious targets set by the UN’s Global Goals: ensuring that no child dies from a preventable disease by 2030. But in 2025, for the first time this century, that progress is set to reverse. Child deaths are, instead, projected to rise — a clear warning sign that hard-won gains in public health are more fragile than most of us would like to believe.
That becomes all the clearer when we consider malaria. Claiming nearly 600,000 lives every year, a child dies from malaria roughly every minute that passes — most of them children under the age of five. While malaria doesn’t have to be a death sentence as it’s both preventable and treatable, it remains an enormous challenge in low- and middle-income countries. It’s particularly entrenched across sub-Saharan Africa, where about 95% of all global deaths from malaria occur.
As it stands, countries around the world are having to reckon with mounting debt cycles, shrinking aid budgets, and resource-intensive crises — leaving little-to-no space to avert these tragic statistics. In fact, for many nations, spending on debt now outpaces spending on health or education. Leading global health officials are being forced to answer a seemingly impossible question: how do you save more lives with less money?
Answers are starting to emerge. Rather than retreating or shrinking ambition, key players are experimenting with ways to make every dollar work harder. A recent agreement between Gavi, the Vaccine Alliance, and UNICEF is set to dramatically lower the cost of malaria vaccines, offering a perfect case study to see that approach in practice.
Let’s take a closer look to see how, even in challenging times, lifesaving progress is still possible.
A Breakthrough Years in the Making
After decades of stalled progress, the world now has multiple malaria vaccines on the scene. Two vaccines — known as RTS,S and R21 — are recommended by the World Health Organization (WHO) and are in the process of being rolled out globally, with a particular focus on Africa. In clinical trials, both have been shown to reduce malaria cases by more than half in the first year after vaccination, with even stronger protection in highly seasonal settings, or places where malaria diagnoses spike during predictably, heavy rainy months.
But scientific breakthroughs alone don’t save lives. Cost, manufacturing, and getting those vaccines in the hands of those who need them matter just as much.
That’s why a recent agreement between Gavi, the Vaccine Alliance, and UNICEF, the world’s largest vaccine buyer, is worth paying attention to. Under the newly announced deal, the price of the R21 malaria vaccine will go for $2.99 per dose, a price drop of about 25%. A significant decrease in this era of trimmed budgets where every dollar counts.
That single price cut is expected to save up to $90 million over the next five years, allowing countries to secure more than 30 million additional doses and protect nearly seven million more children by the end of the decade. That kind of price cut isn’t marginal, it’s life-changing.
How the Deal Works, and Why It Matters
 Pamela Anyango with her child Natasha Aol, 9 months during the the national launch of the malaria vaccine into the routine immunization schedule at Boma Grounds, Apac District, Uganda, in April 2025.©UNICEF/UNI782402
Pamela Anyango with her child Natasha Aol, 9 months during the the national launch of the malaria vaccine into the routine immunization schedule at Boma Grounds, Apac District, Uganda, in April 2025.©UNICEF/UNI782402
UNICEF leverages its enormous bulk-buying power in the vaccine market to negotiate lower prices with manufacturers. Gavi meanwhile helps countries finance the purchase of vaccines and helps integrate them into their immunization programs. Behind the scenes, an innovative financing mechanism — the International Finance Facility for Immunisation (IFFIm) — helps convert long-term pledges from donor countries into immediate cash, allowing Gavi to move quickly when particularly good deals and opportunities arise.
The result: the efficient purchase of huge stockloads by organizations who are global experts in distribution, exactly what’s needed when resources are constrained and health crises loom.
To date, more than 40 million malaria vaccine doses have already been delivered through Gavi-supported programs, with 24 African countries now offering the vaccines as part of routine immunization. Demand is strong: 14 countries introduced malaria vaccines for the first time in 2024, and another seven have followed in 2025.
Uganda, for example, launched Africa’s largest malaria vaccine rollout earlier this year, distributing more than 2.2 million doses across 105 districts to reach over one million children under two-years-old. Zambia and Burundi have also begun national rollouts, while Ethiopia launched one at the very end of 2025. Mali, Guinea, Guinea-Bissau, and Togo are also preparing introductions later this year.
Stretching Every Dollar Further
 Ethiopia rolls out new malaria vaccine integrated with mass distribution of insecticide-treated mosquito nets in Turmi town, South Ethiopia region in September 2025. ©UNICEF Ethiopia/2025.
Ethiopia rolls out new malaria vaccine integrated with mass distribution of insecticide-treated mosquito nets in Turmi town, South Ethiopia region in September 2025. ©UNICEF Ethiopia/2025.
This deal on vaccines reflects a broader shift in global health strategy that we may see more of in the future. With budgets looking thinner, precision matters more than ever to ensure no dollar is wasted. That means moving away from one-size-fits-all campaigns and approaches and assessing the needs of specific countries, cities, and regions on-the ground to make sure their challenges are addressed directly.
To that end, countries are tailoring malaria interventions to the places and seasons with the highest risk. By focusing resources where they have the greatest impact, health systems can layer vaccines with other holistic tools like bed nets, diagnostics, and treatment.
Reducing malaria cases has positive ripple effects that ricochet across an entire society. It frees up hospital beds, strengthens primary health care, and makes hospitals and care facilities overall more resilient to future shocks while also boosting economies by billions.
A Blueprint for What Comes Next
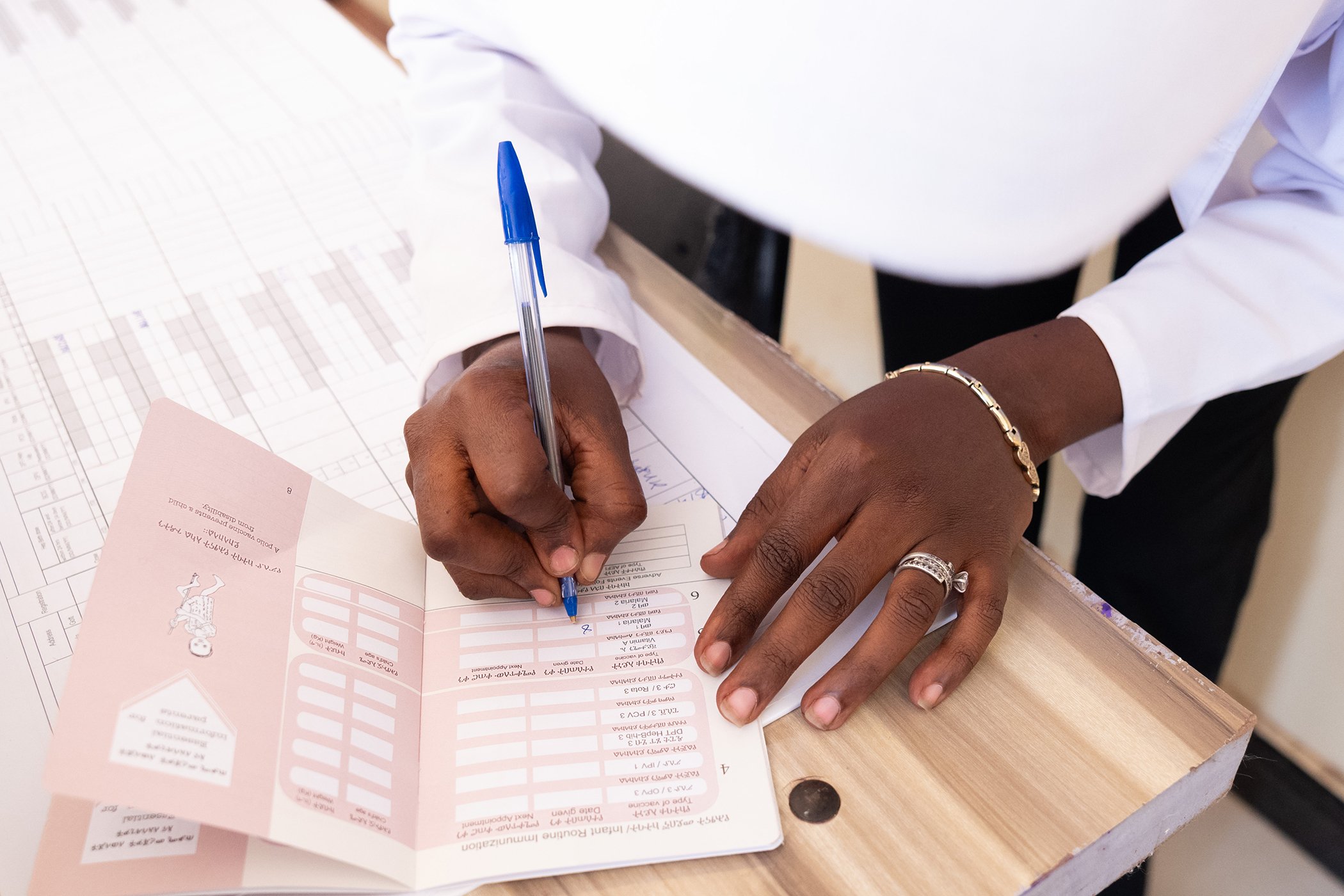
 A health worker shows off a dose of the malaria vaccine during the national launch of the malaria vaccine into the routine immunization schedule at Boma Grounds, Apac District, Uganda, in April 2025.©UNICEF/UNI782402.
A health worker shows off a dose of the malaria vaccine during the national launch of the malaria vaccine into the routine immunization schedule at Boma Grounds, Apac District, Uganda, in April 2025.©UNICEF/UNI782402.
Vaccines remain one of the smartest investments in global health. Since 2000, routine immunization has helped cut child deaths in half, delivering an estimated $54 in benefits for every dollar spent. Yet that statistic alone doesn’t capture the impact of the priceless lives saved by vaccines, more days in school attended, more jobs secured, and more dreams fulfilled because preventable diseases like malaria aren’t able to define the outcome of someone’s life.
However, strides made in global health over the last few decades aren’t guaranteed to stay. When immunization slips, deadly diseases have the chance to return. And the cost of catching up is far higher than the cost of staying on track.
Gavi and UNICEF’s malaria vaccine pricing deal offers a glimpse of what’s possible. It shows that even in a time of uncertainty and limited options, we can still make considerable progress in the road ahead.
It’s important to remember that the world remains close to ending preventable child deaths, despite funding setbacks. Whether malaria follows the path toward being eradicated or, instead, intensifies will depend on whether global leaders choose to invest in the tools that work.