Comfort Owusuaa remembers being turned away.
"I forgot my card," she says. Her baby had a fever, and her arms were full. "They told me to go back home and bring it."
In rural Ghana, a missing outpatient department (OPD) card isn't just a bureaucratic hiccup. It can mean the difference between receiving care and going without. For too long, paper-based records — handwritten, fragile, easily lost — have created a system where access is uncertain. Although this mother’s experience may not happen to every patient, it does happen. But now, something is shifting.
"When I came and they scanned my face," Owusuaa says, "they found my folder quickly. Even if I forget the card now, they can see me.”
What she's describing is more than a technical fix. It's the comfort of knowing that the next time she seeks help, the doors will be open.
From Paper Trails to Digital Presence
Owusuaa is part of a quiet revolution in Ghana's health system — one built on biometric technology. Her face scan connects her directly to her medical history. No card. No guesswork. No delay. This isn't happening everywhere, but in a growing number of rural clinics — now 325 health facilities across the Eastern Region, according to Samuel Laate at Simprints, including the Kotokuom Community-based Health Planning and Services (CHPS) facility — biometric tools like fingerprint and facial scans are helping to solve one of Ghana’s health system gaps: the lack of a universal patient ID.
 Patient health folders on a shelf at the Kotokuom CHPS Compound, Akyemansa District, Eastern Region, Ghana, on July 16, 2025. For too long, paper-based records — handwritten, fragile, easily lost — have created a system where access is uncertain. Image: Nipah Dennis for Global Citizen
Patient health folders on a shelf at the Kotokuom CHPS Compound, Akyemansa District, Eastern Region, Ghana, on July 16, 2025. For too long, paper-based records — handwritten, fragile, easily lost — have created a system where access is uncertain. Image: Nipah Dennis for Global Citizen
The tech comes from Simprints, a nonprofit that builds open-source biometric ID systems for the world's most underserved communities. So far, the system has created around 100,000 unique medical records in Ghana and 800,000 globally for 2024. And it’s no longer a pilot — it’s scaling. By the end of 2025, Simprints aims to reach at least 586 facilities across the Eastern and Oti regions. That’s significant, but still modest in context: According to the 2023 Ghana Health Service (GHS) register, there are about 4,800 registered health facilities nationwide, while Simprints — drawing on the District Health Information Management System 2 (DHIMS2), the national health data platform — counts 11,015 facilities of all types, including smaller, community-based posts.
But the transformation isn't about devices or software. It's about who gets seen, and who gets left behind.
Maternal Health Gaps, Gendered Costs
 Abigail Debrah, 24, on her way to the Kotokuom CHPS Compound in the Akyemansa District, Eastern Region, Ghana, on July 16, 2025. Image: Nipah Dennis for Global Citizen
Abigail Debrah, 24, on her way to the Kotokuom CHPS Compound in the Akyemansa District, Eastern Region, Ghana, on July 16, 2025. Image: Nipah Dennis for Global Citizen
Ghana has made progress in expanding healthcare access, with skilled birth attendance increasing steadily over the past two decades, from 76% in 2014 to 88% in 2022. But structural inequities remain, especially around sexual and reproductive health and rights (SRHR). In rural areas like Akyemansa — located roughly 147 km northeast of Accra, typically a three-hour drive — those inequities can intensify.
"Some women can't afford transportation," says Dr. Koranteng Ampaw, the Akyemansa District Director of Health. "Others can't travel without permission as a result of gender norms and low autonomy among women.”
Without consistent ID, medical histories are scattered. A woman might be logged under three different spellings of her name, in three different clinics. Follow-up is spotty. Misdiagnoses increase. Vaccination records are lost.
“This lack of a unified system presents considerable operational obstacles for healthcare providers… and has particularly grave implications for maternal and child health… the inability to reliably verify a child’s identity disrupts the vaccination schedule, leaving children vulnerable to preventable diseases,” says Laate, Senior Country Manager at Simprints. “In cases where clients have been enrolled using Simprints’ biometric technology, healthcare workers can immediately and accurately retrieve their electronic health records. From the patient’s perspective, it eliminates a critical barrier to care… increasing service completion rates, and minimizing resource wastage.”
Faster Isn't the Whole Story
Abigail Debrah sees it on the ground. "Before, I forgot my child's card and they couldn't find her in the book," she says. "Now they scan my face and everything is there. I don't stay long anymore."
But this isn't just about time. For Debrah, it's about dignity, being recognized. Being remembered. Knowing that even if a piece of paper gets lost, the system still knows who she is.
 Nurse Zainab Abdullahi (right), 29, a community health nurse, verifies the identity of Abigail Debrah (left), 24, using the Simprints biometric system at the Kotokuom CHPS Compound, Akyemansa District, Eastern Region, Ghana, on July 16, 2025. Image: Nipah Dennis for Global Citizen
Nurse Zainab Abdullahi (right), 29, a community health nurse, verifies the identity of Abigail Debrah (left), 24, using the Simprints biometric system at the Kotokuom CHPS Compound, Akyemansa District, Eastern Region, Ghana, on July 16, 2025. Image: Nipah Dennis for Global Citizen
Nurse Zainab Abdullahi agrees. "Before, if a patient didn't have their card, we'd search registers for a long time," she says. "Now, we scan them. We find their records quickly. We can follow up, see which vaccines are due, even visit them if they miss an appointment."
There was skepticism at first. Some patients didn't trust the tech. "They asked if we were using their photos for something else," Abdullahi recalls. "But once they saw how it helped them, they wanted to enroll."
Trust isn't built by asking people to believe in the system. It's built when the system works.
Digital Tools Supporting Ghana’s Health System
Of course, tech isn't a silver bullet. Ghana's rural clinics are chronically under-resourced. A 2019 study of primary healthcare facilities found that nearly one-third had no electricity at all, and only 29% of those with power could depend on it. While the study doesn’t isolate rural clinics, healthcare workers say those in outlying areas are often the hardest hit. Without consistent electricity, safe storage of vaccines and temperature-sensitive vaccines becomes nearly impossible.
"When the system works, it's powerful," says Benjamin Somuah, Akyemansa District Health Information Officer. "But when infrastructure fails, we risk running both paper and digital systems at once. That slows us down."
Questions of data ownership, consent, and sustainability are not hypothetical — they’re make-or-break. Simprints tackles these head on: consent is documented at every step, no identifiable data is stored, and systems meet both Ghanaian laws and the European Union’s General Data Protection Regulation (GDPR) standards. But technology alone won’t guarantee success. As Laate puts it, “If there is no genuine commitment to capacity building and a clear path to government ownership, the solution collapses the moment NGO funding ends. That’s how you end up with a pilot graveyard.”
High privacy standards and community-led rollouts are necessary, but not sufficient. National scale demands more: policy frameworks, long-term budgets, and sustained political will.
"Biometric health ID should be part of Ghana's national health strategy," Dr. Ampaw says. "We need to move from pilots to permanent infrastructure. Otherwise, it won't last."
The Right to Be Found
Behind the policy and infrastructure are mothers like Owusuaa and Debrah, women whose strengths have sustained them through gaps that new technology is only now beginning to fill.
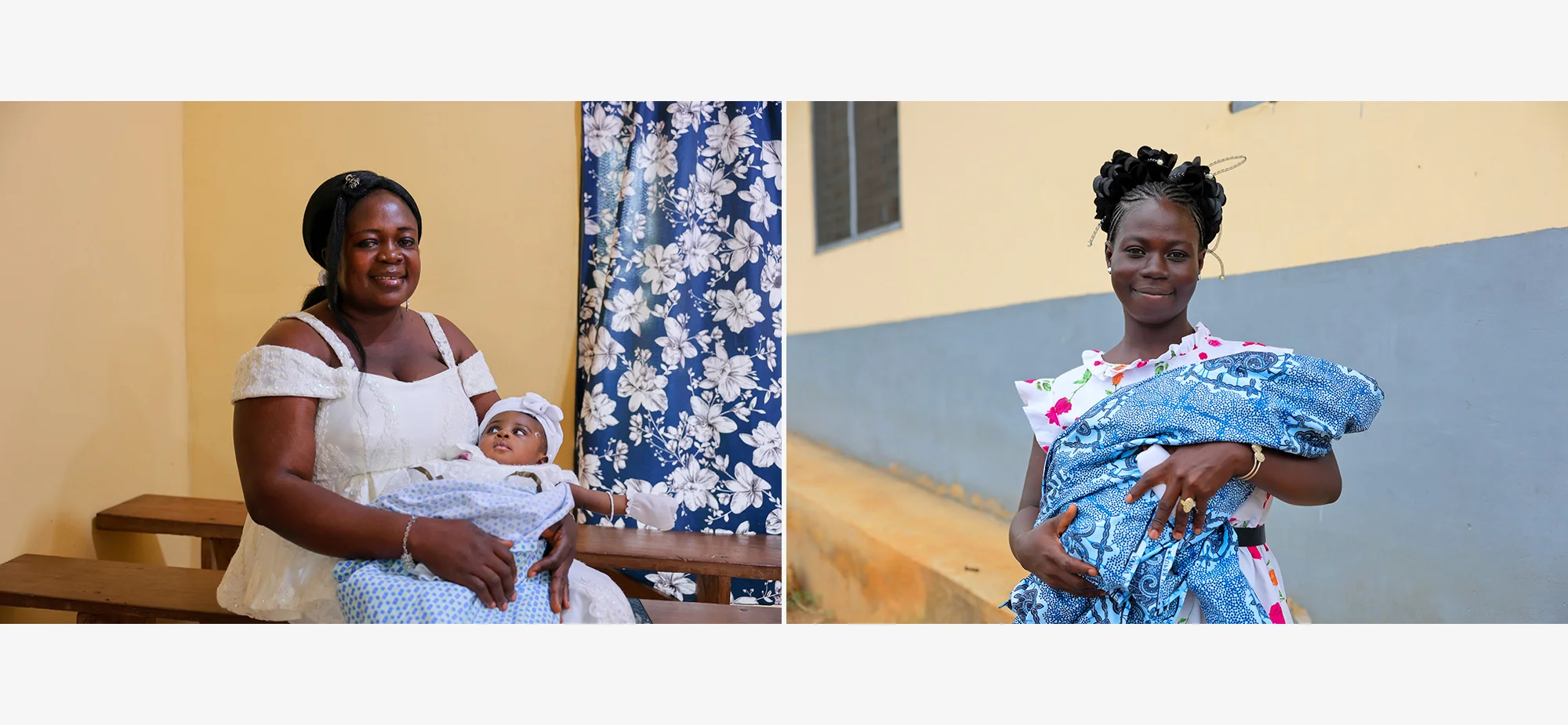 Comfort Owusuaa (left), poses for a portrait with her daughter and Comfort Sarpong (right), poses for a portrait with her child, both at the Kotokuom CHPS Compound in the Akyemansa District, Eastern Region, Ghana, on July 16, 2025. Image: Nipah Dennis for Global Citizen
Comfort Owusuaa (left), poses for a portrait with her daughter and Comfort Sarpong (right), poses for a portrait with her child, both at the Kotokuom CHPS Compound in the Akyemansa District, Eastern Region, Ghana, on July 16, 2025. Image: Nipah Dennis for Global Citizen
Now, they're seen quickly, and with biometric patient ID, a forgotten card doesn’t cause any delays. Their children are getting vaccinated. Their records are intact. And most importantly, they are known.
If we're serious about improving maternal health in places like rural Ghana, we need more than service delivery. We need the systems, the digital backbone, the human labor, the public trust, that make care continuous.
That means investing in tools like biometric ID. It means training health workers. It means making sure women don't just get care once but are seen and remembered every time.
We often say no one should be left behind. But to make that real, we need to prioritize systems that reach everyone, no matter where they live.
Biometric ID isn't a shiny fix; it's a building block. Governments and donors across the African continent must treat solutions like these as long-term public infrastructure, not a pilot project. When women are recognized, care gets faster, safer, and more humane. Their right to health becomes visible on record, and in reality.
 Abigail Debrah, 24, with her daughter at the Kotokuom CHPS Compound in the Akyemansa District, Eastern Region, Ghana, on July 16, 2025. Image: Nipah Dennis for Global Citizen
Abigail Debrah, 24, with her daughter at the Kotokuom CHPS Compound in the Akyemansa District, Eastern Region, Ghana, on July 16, 2025. Image: Nipah Dennis for Global Citizen
Editor’s Note: This article is part of a content series that was made possible with funding from the Susan Thompson Buffett Foundation.

